Policy number: SRP 068
Policy name: Knee Joint Replacement
Status: Group Prior Approval
Effective date: 1 April 2024
Next review date: 1 April 2026
Mid and South Essex ICB commission surgery for Knee Joint Replacement on a restricted basis.
Referral for consideration of elective knee joint replacement surgery should only be made when the patient has intense or severe joint symptoms (pain, stiffness and reduced function) that have a substantial impact on their quality of life AND are refractory to non-surgical treatment* for at least 6 months AND has radiological features of severe disease. Plain radiographs, with standing AP (or long-leg) and a lateral view may be taken for initial diagnosis but are not essential in patients over 45. Skyline and Rosenberg views may also be requested. Note that standard radiographs are required on all patients prior to referral to secondary care.
*Non-Surgical Treatment – Prior to referral patients must have received and engaged in all core non-operative treatments AND at least one additional non-operative therapy for at least 6 months.
Core treatments for all patients:
- Accurate verbal and written information to enhance understanding of the condition and its management and to counter misconceptions, such as that it inevitably progresses and cannot be treated. Ensure that information sharing is an ongoing, integral part of the management plan rather than a single event at time of presentation.
- Exercise irrespective of age, comorbidity, pain severity or disability. Exercise should include local muscle strengthening and general aerobic fitness.
- Interventions to achieve weight loss if the patient is overweight. Weight maintenance also has a role in managing symptoms.
- Advice on appropriate footwear (including shock-absorbing properties).
- Individualised self-management strategies with the person with osteoarthritis. Ensure that positive behavioural changes, such as exercise, weight loss, use of suitable footwear and pacing, are appropriately targeted.
- Additional non-operative therapies include manual therapy (e.g. physiotherapy), supports and braces, local heat and cold therapy, non-steroidal anti-inflammatory medication (topical or oral) or COX-2 inhibitors with a proton pump inhibitor, opioid medication, and intra-articular corticosteroid knee injections.
The Oxford Knee Score should be completed in Primary Care prior to referral for consideration of surgical knee joint replacement. The completed tool in full (not just the score) should be attached to the referral. The tool can be found at: http://www.orthopaedicscore.com/scorepages/oxford_knee_score.html
The Oxford Knee Score tool should be used in conjunction with other information to help a patient make a sensible decision as whether to proceed to surgery or not. This, together with the Shared Decision Making Support Tool- Deciding what to do about osteoarthritis of the knee – should form the basis for this discussion between GP/triage referral service and patient.
Grading for the Oxford Knee Score
0 -19 May indicate severe knee arthritis. It is likely that some form of surgical intervention is required- Offer referral to a consultant orthopaedic surgeon for consideration of knee surgery.
20 – 29 May indicate moderate to severe knee arthritis. Consider seeking advice and guidance (eRS) from consultant orthopaedic surgeon.
30 – 39 May indicate mild to moderate knee arthritis. Patients may benefit from non-surgical treatment, such as exercise, weight loss, and /or anti-inflammatory medication.
40 – 48 May indicate satisfactory joint function. May not require any formal treatment
MSE ICB will only fund knee joint replacements if:
- The patient complains of intense or severe symptomatology AND has radiological features of severe disease AND has demonstrated disease within all three compartments of the knee (tri-compartmental) or localised to one compartment plus patello-femoral disease (bi-compartmental).
OR
- The patient complains of intense or severe symptomatology AND has radiological features of moderate disease AND limited mobility, or stability of the knee joint is severely impacting on activities of daily living. Information demonstrating the severity of the impact on activities of daily living must be included in the referral letter.
*Please refer to the table overleaf for classification of pain levels and functional limitations to comply with policy.
In all cases:
- Shared decision making must take place with respect to all management. This includes presenting the patient with information on all treatment options, and a clear description of the risks and benefits of each treatment, including surgery where indicated. Emphasis should be on dialogue enabling patients to realise they have a choice, understand the options available to them, and make a decision as to which option to choose.
- Evidence that the patient has been fully involved in the decision to have joint surgery and including evidence of shared decision making i.e. a full record of the discussion with the patient in their hospital notes and including risk/benefits of all treatment options offered.
- There must be documented supporting clinical diagnostics and other assessments to support the decision to perform joint surgery.
Knee Joint Replacement – Classification of Pain Levels and Functional Limitations
| Variable | Definition |
| Mobility and Stability | |
| Preserved mobility and stable joint | Preserved mobility is equivalent to minimum range of movement from 0o to 90o. Stable or not lax is equivalent to an absence of slackness of more than 5mm in the extended joint. |
| Limited mobility and/or stable joint | Limited mobility is equivalent to a range of movement less than 0o to 90o unstable or lax is equivalent to the presence of slackness of more than 5mm in the extended joint. |
| Symptomatology | |
| Slight | Sporadic pain. Pain when climbing/descending stairs. Allows daily activities to be carried out (those requiring great physical activity may be limited). Medication, aspirin, paracetamol or NSAIDs to control pain with no/few side effects. |
| Moderate | Occasional pain. Pain when walking on level surfaces (half an hour or standing). Some limitation of daily activities. Medication, aspirin, paracetamol or NSAIDs to control with no/few side effects. |
| Intense | Pain of almost continuous nature. Pain when walking short distances on level surfaces or standing for less than half an hour. Daily activities significantly limited. Continuous use of NSAIDs for treatment to take effect. Requires the sporadic use of support systems walking stick, crutches). |
| Severe | Continuous pain. Pain when resting. Daily activities significantly limited constantly. Continuous use of analgesics – narcotics/NSAIDs with adverse effects or no response. Requires more constant use of support systems (walking stick, crutches). |
| Radiology | |
| Slight | Ahlback grade I. |
| Moderate | Ahlback grade II and III. |
| Severe | Ahlback grade IV and V. |
| Localisation | |
| Unicompartmental | Excluded patello-femoral isolated. |
| Bicompartmental | Unicompartmental plus patello-femoral. |
| Tricompartmental | Disease affecting all three compartments of the knee. |
MSE ICB commission Primary Knee Replacements based on good clinical practice pathways as identified by the British Orthopaedic Association and Monitor1.
The ICB commissions knee replacement in line with the British Orthopaedic Association good practice pathway:
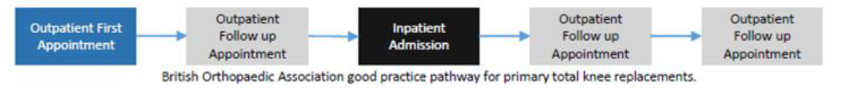
Defined as:
- a first outpatient appointment,
- a follow-up outpatient appointment,
- an inpatient admission and
- two outpatient follow-up appointments maximum only.
Further long-term routine ongoing follow up is considered to be a low clinical priority and not routinely funded.
Funding for patients not meeting the above criteria will only be granted in clinically exceptional circumstances.
Individual funding requests should only be made where the patient demonstrates clinical exceptionality.
Find out more information on applying for funding in exceptional clinical circumstances
Reference:
NICE NG226 Osteoarthritis in over 16s: diagnosis and management www.nice.org.uk/Guidance/NG226