Consultation dates: 25 January to 11 April 2024
On this page
- About this document
- About this consultation
- Which services are included in this consultation?
- How to respond – we need your views
- Who should read this document?
- How do I use this document?
- What is not included in our consultation?
- Introduction – The background to this consultation
- Public, patient and staff involvement
- Why we should change
- The condition of St Peter’s Hospital, Maldon
- How we developed our proposals
- Consultation proposals
- Staffing, equality and health inequalities issues
- Have your say
- What happens next
About this document
This document outlines our public consultation into services at local community hospitals. We are gathering views and ideas on:
- our proposals for potential changes to the locations where we provide some of our inpatient services for community hospital intermediate care and stroke rehabilitation, and freestanding midwife-led birthing services; and
- the possibility of moving all other patient services at St Peter’s Hospital, Maldon to other locations, mostly in and around Maldon.
We’ve set out our proposed changes in the consultation proposals section that starts on page 20 of this document. There are lots of ways to comment on them.
If you need this document in another language or another format such as large print or audio please call 01268 594350 or email [email protected]
About this consultation
This consultation is being run by Mid and South Essex Integrated Care Board (ICB). This is the organisation responsible for planning and paying for NHS health and care services for the 1.2 million people living across mid Essex, south east Essex, Basildon and Brentwood, and Thurrock.
The ICB is committed to delivering local, high quality healthcare services while making sure we achieve the best value for money and equity of access for our growing population.
This consultation document sets out:
- The background to our proposals
- Our proposals
- The current situation in each of the service areas
Our proposals are:
- To change how and where people receive inpatient intermediate care services and stroke rehabilitation inpatient services that are provided from community hospitals.
- To make permanent the relocation of a freestanding midwife-led birthing unit from St Peter’s Hospital, Maldon to the William Julien Courtauld Birthing Unit (WJC) at Braintree Community Hospital.
- And, we’re asking for views on the possibility of moving all the other patient services provided at St Peter’s Hospital, Maldon to other locations in and around Maldon.
If all these proposals are agreed, it will mean that all the NHS services provided at St Peter’s Hospital in Maldon will be moved to other sites. After that it is likely that Mid and South Essex NHS Foundation Trust and Essex Partnership University NHS Foundation Trust, who own the site, will decide to close St Peter’s Hospital permanently and sell the site. The money from the sale would go back to the NHS in mid and south Essex. The proposals that we are describing in this document are just that: proposals. We are asking local people to share their thoughts before we decide what to do. We will consider your responses carefully and take them into account when we’re making decisions about these proposals.
This consultation document acts as a summary of our full pre-consultation business case (PCBC), which is a large technical document. You can read that document and other information for the consultation on the consultation website.
Which services are included in this consultation?
These FOUR services are included in this consultation:
Intermediate care inpatient services
Most people go straight home after treatment and care at an acute hospital. Some people need a short, additional stay in a community hospital to help them get better before they can go home. These services provide that support. Most of the people who need this support are in the older age groups. Sometimes these services admit people who are unwell, but not in need of treatment at a bigger hospital. How many people need these services in mid and South Essex each year? Approximately 2,080
Stroke rehabilitation inpatient services
Lots of stroke patients go straight home after receiving emergency treatment for a stroke at one of our bigger hospitals, and get their rehabilitation support at home or in community clinics. Some people will need an additional stay in a community hospital to receive specialist rehabilitation services. Patients get an individually tailored programme of rehabilitation support from physiotherapists, occupational therapists, speech and language therapists and other services to aid their recovery. Stroke rehabilitation inpatient services can also benefit a small number of people with some types of other brain injury caused by an accident or illness. How many people need these services in mid and South Essex each year? Stroke rehabilitation inpatient services
Freestanding midwife-led birthing unit
A freestanding midwife-led birthing unit is staffed by midwives and maternity support workers. They care for healthy women expecting straightforward pregnancies during labour and following birth. The units are in community settings, often in community hospitals. If women or babies need specialist medical or neonatal care, they need to be transferred by ambulance or car to a doctor-led maternity unit at a bigger hospital. How many people used the freestanding midwife-led birthing unit at St Peter’s Hospital? Last year 6 births/month on average and 77 births in 2022/23. The service had to be closed several times because there weren’t enough staff available to run it safely.
Other patient services provided at St Peter’s Hospital, Maldon
These are services for people who don’t need to stay in hospital overnight. This includes outpatient services, prenatal and postnatal clinics, the Cherry Trees Therapy Centre for mental health patients, podiatry clinics, X-rays, ultrasound scans, and blood tests. How many people use these services each day on average? 250 – 300.
How to respond – we need your views
There are different ways to get involved in the consultation and give your views. We want to make it as easy as possible for you to tell us what you think of the proposals.
- Attend a public meeting: There are different types of events planned during the consultation period at different times, days of the week and locations both in person and online. People are asked to register in advance simply to ensure the events are well staffed and managed to provide the best experience for everyone and to make sure views are captured. Further information about these events can be found on page 34 this document.
- Give evidence or attend the public consultation hearing We will be holding a public consultation hearing. This is an event that gives people the opportunity to present evidence or tell us their views on the proposals directly. People can also come along to hear what is happening or view online live during the hearing or view a recording afterwards. More information about the public consultation hearing and how to get involved is included at the back of this document.
- Voluntary and community sector groups will be running events and holding focus groups for service users and carers most likely to be impacted by any proposed changes. If you would like to get involved in these activities then please let us know.
- A consultation survey is available online via the website as well as paper copies available at libraries and some other public venues. Please check our website for exact locations. You can also request a paper copy by contacting us and we will send one to you. If you need help to fill in the survey please contact us and we will be happy to arrange some support for you.
- Individual or organisational responses and submissions: We welcome responses from individuals or organisations. Please make sure they are submitted before the end of the consultation. When you respond to the consultation, please include your reasons for the responses you give. If you can include good explanations and even share evidence that backs the points you make, that will really help us understand your response.
- Join the conversation on Virtual Views, the Mid and South Essex online engagement hub.
- Email us [email protected]
- Contact us via social media https://www.facebook.com/MSEICS/ https://x.com/MSEssex_ICS
- Telephone: 01268 594350
- Write to us: FAO: Community Capacity Consultation NHS Mid and South Essex ICB, PO Box 6483, Basildon, SS14 0UG
Who should read this document?
The information in this document is for anyone who lives or works in the area, has experience of or an interest in:
- the care we provide to people who need a stay in one of our community hospitals for intermediate care or stroke rehabilitation after being treated at one of our bigger hospitals.
- midwife-led birthing services provided in mid and south Essex;
- the services we provide at St Peter’s Hospital, Maldon for people who don’t need a stay in hospital. Services like outpatient clinics, antenatal and postnatal clinics, physiotherapy, mental health services, and diagnostics services like x-ray, ultrasound scans, or blood tests.
The information is also intended for people who use services provided by Mid and South Essex NHS Foundation Trust, Essex Partnership NHS Foundation Trust, Provide Community Interest Company and North East London NHS Foundation Trust. It doesn’t matter if you have previously used these services or not, we would like to hear your views on the potential changes to these services in your area.
How do I use this document?
This document aims to give you the information you need to understand and respond to our proposals. As you read it, you’ll find out about the challenges we’re working on, and why we think we need to change. We explain how we arrived at our proposals, and how we involved the people that use, work in and rely on the services. And we set out the proposals for changes to services that we’re asking for your thoughts and comments on, and how you can take part and respond. We suggest you read the introduction and each of the sections you are interested in. You can respond to one, some, or all our proposals. As you go through this document, you’ll see notes telling you where you find more information, if you need it. More documents and information is available on our website.
What is not included in our consultation?
This consultation does not affect:
- he emergency stroke care that only our bigger hospitals in Southend, Basildon and Chelmsford can provide.
- The support to live independently with or following an illness and rehabilitation services that we provide to patients at home, in residential care places, and in community clinics.
- The intermediate care services provided by Essex County Council, Southend-on-Sea City Council, and Thurrock Council, or
- St Peter’s Court care home, next to St Peter’s Hospital, Maldon.
Introduction – The background to this consultation
We started thinking about how community hospital beds could give more patients the support they need several years ago. We moved some of those services around in the COVID-19 pandemic to keep our staff and patients as safe as possible. That meant some patients went to hospitals that they wouldn’t normally expect to go to. We gradually moved those services back to where they had been. In 2022, we asked an independent panel of doctors and other specialists for their professional view on our ideas on how to make better use of our community hospitals. In 2023, it became clear that we needed more community hospital beds for patients who need stroke rehabilitation support. We had room for 16 stroke rehabilitation patients at St Peter’s Hospital in Maldon and 8 at the Cumberlege Intermediate Care Centre in Rochford.
The building at St Peter’s Hospital in Maldon is in poor repair. That means parts of it are no longer safe for patients to stay in or staff to work in, and we had to think carefully about how to arrange our services to support more patients safely this winter. The Bayman Ward at Brentwood Community Hospital is in good condition and has capacity for 25 inpatients, nine more than St Peter’s Hospital, so we moved our stroke rehabilitation services from Maldon to Brentwood. And we increased the stroke rehabilitation capacity at the Cumberlege Intermediate Care Centre in Rochford from 8 patients to 14 patients. That reduced intermediate care capacity in Rochford from 14 patients to 8.
- 2019 Pre COVID-19 review of contribution and performance of community beds to improve patient outcomes
- 2021 Emergency changes during COVID-19 to keep people safe
- 2022 Review of clinical model and distribution
- 2023 Urgent winter changes to ensure patient safety and flow
- 2024 A taskforce of local doctors, nurses, and other service leaders prepare options for public consultation
Those changes mean that at any one time in our community hospitals this winter (2023-24) we can support:
- 39 99 stroke rehabilitation patients. That’s 15 more than we could before taking this decision, and still short of the 48-50 beds we think we need.
- 99 patients needing intermediate care. That’s 6 less than we could before taking this decision and still more than the 77-87 beds we think we need.
Our aims
- Improve outcomes in population health and healthcare
- Tackle inequalities in outcomes, experience and access
- Enhance productivity and value for money
- Support broader social and economic development
Public, patient and staff involvement
NHS Mid and South Essex Integrated Care Board has a continuous programme of engagement. In November and December 2023, we talked with patients, carers, community groups, local residents and staff about:
- Future configuration of inpatient NHS intermediate care beds and inpatient stroke rehabilitation beds.
- Midwife-led birthing care
- Other services provided at St Peter’s Hospital, Maldon
Local people participated in two online surveys, and a mix of 20 in-person and online focus groups across the area. NHS staff took part in 10 more focus groups.
Some of the topics explored during these sessions included:
- What does great care look and feel like to you?
- What works well in the services you or your loved one have experienced?
- What is not working so well now and why do you think that is?
- What one thing should we change to improve your experience?
We also shared and discussed some of the thinking about potential decision-making criteria that we could use to help narrow down the potential options.
A report of the engagement exercise was completed independently and its findings endorsed by Healthwatch Essex and Healthwatch Southend, independent bodies that represent the views of local people who use health and social care services in our area.
The importance of community-based provision was emphasised throughout the engagement period. Patients, community groups and staff are extremely passionate about the provision of community-based services and the need to ensure that they are well maintained, and evolving to serve the needs of the changing population.
When asked in the survey “what about your care is most important to you?”, the responses highlighted the following ranking (1 being ranked the most important and 7 the least):
- Right treatment at the right time
- Access to the best clinical treatment
- Ease of access
- Specialist centre for your condition
- Enough staff on duty
- Family and friends close by
- Quality of building where care is delivered.
The themes highlighted by participants create an opportunity for simple recommendations to be implemented to make sure patients, community groups and staff continue to work together to help the people of mid and south Essex live longer and healthier lives. These recommendations include:
- Good communication and engagement – the importance of simple and clear messaging being consistently provided to avoid misunderstandings and misinformation was a theme common to all participants. Also ensuring good communication within and between the wider health and care system – including acute hospital, primary and social care.
- Focus on equity and inclusion – ensure that the consultation is wide reaching and inclusive.
- Accessibility – minimising waiting times, and geographically; focus on local-based solutions where possible, making it easier for carers, friends and family to visit.
- Patient choice – support initiatives that continue to maximise patient choice. This may require alternative solutions to be developed but this is encouraged and welcomed by staff and patients.
- Involving patients in care planning – the importance of patients and carers being very involved in care. For example, care planning with each patient and their family, promoting independence by training carers and family members and developing personal goals and outcomes.
- Transitioning from hospital – the value of community beds as an important part of a transition from hospital to returning home, and providing a setting in which care can be much more personalised.
- The right staff – community beds are increasingly used for people with greater needs, resulting in a strong emphasis on having the right staff with the right skills.
Involving our staff
Staff associated with community inpatient beds We invited all staff working on wards in the community hospitals, and staff in related services, like the Recovery at Home team and stroke teams working in the main hospitals, to share their views. People could have their say via focus groups and using an online tool.
Areas explored included:
- What is important to your patients and their carers and why?
- What enables you to deliver great care?
- What are the barriers to delivering great care?
- If you could change one thing about the provision of community beds, what would it be?
Things that staff said were important included:
- Delivering care as close to the patient’s home as possible.
- Clear communication with staff so they can support the continuity of patient care. Good transport links to health and care services for family, carers, friends and staff. The critical role families and loved ones play in patient recovery, and the need to involve them in decision-making and care planning.
- Continuing to improve links with social care to ensure services are integrated. Access to regular, good quality therapy services to support rehabilitation.
- Trained, skilled staff available at all times, and improved access to learning and training.
- Care should be personalised, needs-based and not restricted by rigid pathways or procedures.
Staff associated with maternity services
The staff associated with maternity services shared common themes with those working with community bed services. Themes particular to maternity included:
- The importance of patient choice; supporting women and birthing people to have the birth experience they desire.
- Consistent staffing levels that deliver equitable outcomes for women and birthing people.
- The importance of ring-fenced staff to create a network of support around families.
Staff associated with other patient services at St Peter’s Hospital
We spoke with staff working in non-inpatient areas at St Peter’s Hospital for their views to help shape proposals. The same themes arose as with other staff groups, with the addition of the importance of providing a homely environment with modern well-equipped facilities to deliver the best possible experience for patients. The full findings from this engagement exercise are available on our website.
Why we should change
Community hospital intermediate care services
More people are living in mid and south Essex. And thanks to advances in medicines and treatments more people are living longer. That means lots more people over the age of 75 are living in the area. This older population is more likely to live with more than one long-term medical condition. That means there are more patients for our hospitals to treat and care for. Older people are more likely to need to go to hospital and they are more likely to take longer and need more support to recover. People over 75 are the main users of community hospital beds where they receive care to help them recover before going home. The care people receive from some of these services in our area doesn’t meet national standards. Improving these services will mean people recover more fully and more quickly. It’s important we make sure everyone gets good care wherever they live in our area. Community hospitals are one part of our health and care system. They work with our bigger hospitals at Southend, Basildon and Chelmsford, with GP, pharmacy and other primary health care, social care, and a whole range of community health services.
We are developing new services all the time. We have introduced:
- virtual wards, technology that helps patients to manage their care at home, and
- transfer of care hubs, which coordinate care and support for patients who need it.
These new approaches aim to make sure patients get out of hospital more quickly, recover more quickly, and get back home more quickly. Between April and August 2023 the NHS in mid and south Essex was the best in the country at getting patients back home, or to other appropriate care settings after treatment in an acute hospital. That’s because we have worked hard since 2022 putting in place Urgent Community Response Teams, admission avoidance, Early Discharge Services (EDS), and Integrated Discharge Teams (IDTs). This has shown us that a variety of community health and care interventions are needed.
These new approaches aim to make sure patients get out of hospital more quickly, recover more quickly, and get back home more quickly.
Between April and August 2023 the NHS in mid and south Essex was the best in the country at getting patients back home, or to other appropriate care settings after treatment in an acute hospital. That’s because we have worked hard since 2022 putting in place Urgent Community Response Teams, admission avoidance, Early Discharge Services (EDS), and Integrated Discharge Teams (IDTs). This has shown us that a variety of community health and care interventions are needed.
National guidance tells us that of the patients discharged from an acute hospital:
- 50% should be able to go home without further support
- 45% should be able to go home with some further support
- 4% are likely to need a short stay in a community hospital or a residential care home, depending on the type of support need
- 1% will need to be accommodated where their needs can be met, such as in a care or nursing home
National Intermediate Care Pathway Guidance
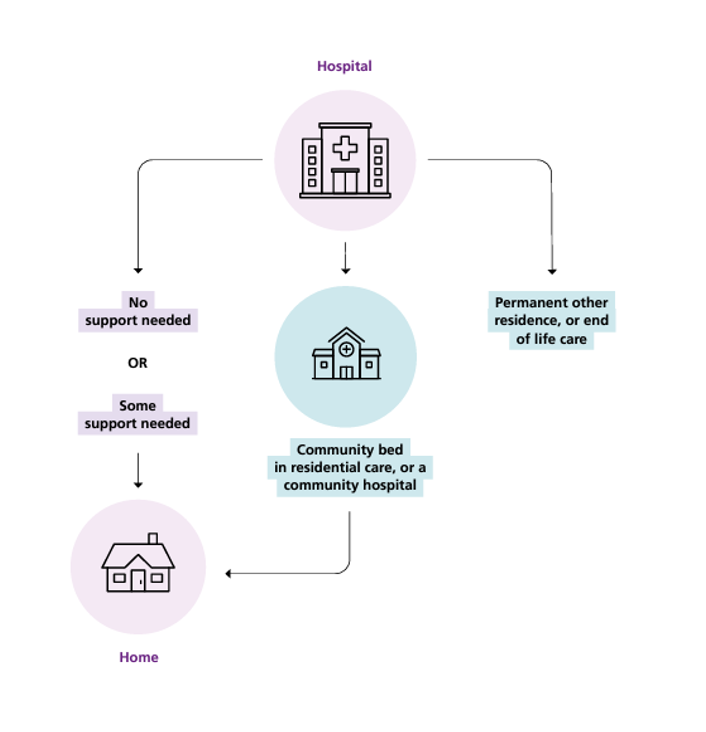
National Intermediate Care Pathway Guidance
Diagram depicting a large hospital with three discharge routes. Left: Home with or without rehabilitation support. Right: New permanent residence or end-of-life care. Middle: Short stay in community hospital or residential care home, then return home.
We have calculated that we need between 77 and 87 beds in our community hospitals for these patients if:
- 4% of patients discharged from an acute hospital need a community bed,
- This population is set to increase by 8% in the next five years,
- The average time patients need in a community hospital stays the same, 95% of those beds are used at any one time,
- Current local authority intermediate care bed capacity in each of Southend, Thurrock and Essex County Councils is appropriately used.
To make sure everyone has the best possible chance of getting the care they need, recovering well, and getting home as quickly as possible, we need to change some of the places where we provide inpatient intermediate care.
Inpatient stroke rehabilitation services
The injury to the brain caused by a stroke can lead to widespread and long-lasting problems. Some people recover quickly. Others need longer-term support to help them regain as much independence as possible. Rehabilitation support can be provided at home, at clinics near home or in a hospital or community hospital setting. A specialist unit would include physiotherapists, psychologists, occupational therapists, speech and language therapists, dietitians, and specialist nurses and doctors.
Some of the patients needing specialist stroke rehabilitation in a dedicated community hospital will be younger than patients who need a stay for intermediate care. Our own information shows that stroke patients in our area don’t do as well as similar patients in other areas. Our doctors, nurses and service leaders have calculated that we need dedicated, specialist spaces for 48-50 stroke rehabilitation patients in our community hospitals if we are to offer spaces to everyone who would benefit and help more people recover more fully.
Stroke service model
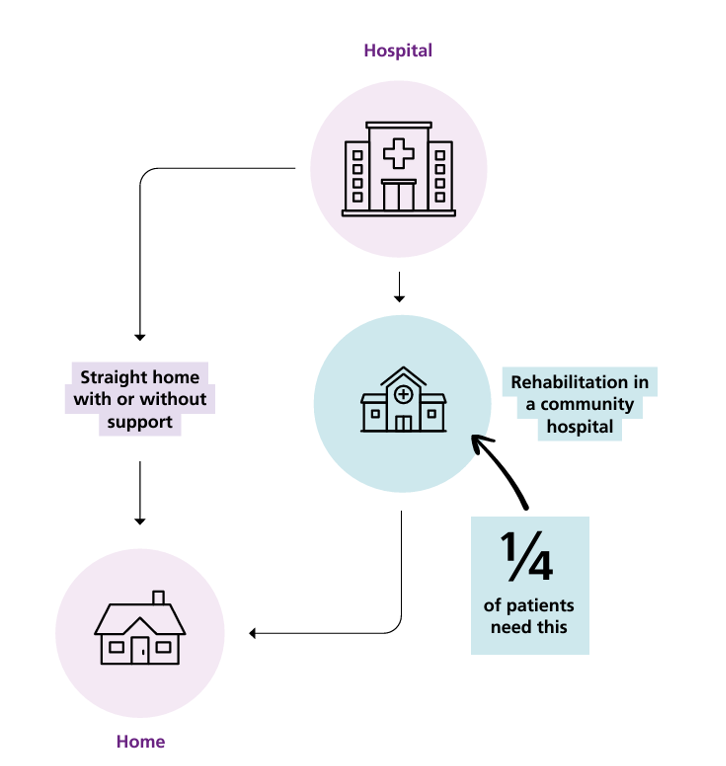
Stroke service model
Hospital process diagram: Stroke patients have two discharge routes. Left: Home with or without rehab support. Right: Rehab in community hospital, then return home. One quarter of patients require community hospital rehab
If a patient who has had a stroke would benefit from rehabilitation that can’t be provided in their own home, they might be eligible for a stay in a community hospital stroke rehabilitation unit (SRU). There they will have intensive support to help them recover as fully as possible. As soon as it is possible for rehabilitation to be continued in their own home that will be arranged. Usually a stay in a community stroke rehabilitation unit could be up to 6 weeks. How long someone stays in hospital depends on their needs.
In mid and south Essex, more patients than we have space for need a stay in a community hospital for specialist rehabilitation support after a stroke. That means some patients have to stay in a bigger hospital waiting for a specialist rehabilitation space to become available, or go to rehabilitation services outside the area. At the moment, the stroke rehabilitation services we provide in our community hospitals don’t have enough staff to meet national requirements.
Creating a specialist stroke rehabilitation centre, or centres would allow us to increase the number of stroke patients we can support. That means we will be able to give all our stroke patients who need it the expertise and intensity of rehabilitation support they need as soon as they need it. And specialist stroke centres are a more attractive option for clinical staff when they are choosing where to apply for jobs.
Bringing specialist stroke services together would have benefits for people needing rehabilitation support for some other brain injuries caused by an accident or an illness like encephalitis or meningitis. A larger specialist stroke unit would mean some of these patients would be able to stay in the area to get the specialist support they need. Patients with the most complex of these brain injuries will still have to travel outside mid and south Essex for their rehabilitation support.
Having more stroke rehabilitation beds in our community hospitals, will mean more stroke patients can benefit from access to specialist rehabilitation following emergency treatment as soon as their medical team says they are ready.
Bringing specialist stroke services together would have benefits for people needing rehabilitation support for some other brain injuries caused by an accident or an illness like encephalitis or meningitis. A larger specialist stroke unit would mean some of these patients would be able to stay in the area to get the specialist support they need. Patients with the most complex of these brain injuries will still have to travel outside mid and south Essex for their rehabilitation support. Having more stroke rehabilitation beds in our community hospitals, will mean more stroke patients can benefit from access to specialist rehabilitation following emergency treatment as soon as their medical team says they are ready.
Freestanding midwife-led birthing unit
We offer a choice of services and locations for giving birth in mid and south Essex.
- At a doctor-led, hospital maternity unit (Southend, Chelmsford, and Basildon) – people are looked after by midwives in a doctor-led unit. There is fast access to doctors and other medical support, if there are any complications during the birth.
- At a midwife-led birthing unit at a hospital that has a doctor-led maternity unit (Southend, Chelmsford, and Basildon) – people are looked after by midwives and maternity support workers. The hospital’s doctor-led maternity unit is very close by, if there are any complications during the birth.
- At a freestanding midwife-led birthing unit. (A unit that is not at a hospital with another maternity service) (Maldon) – people are looked after by midwives and maternity support workers. Service users would need to be transferred by ambulance or car to a hospital maternity unit, if there are any complications during the birth.
- At home – people can give birth with support from a midwife. If service users need any help or their labour is not progressing as well as it should, the midwife will arrange for them to go to hospital.
In August 2023, we decided to move midwife-led and low-risk births from St Peter’s Hospital in Maldon temporarily to the unused William Julien Courtauld (WJC) Birthing Centre at Braintree Community Hospital. The freestanding midwife-led birthing unit at St Peter’s Hospital has been closed several times because there weren’t enough staff available to run it safely. And the poor condition of the buildings has affected the quality of care we can provide there.
Moving inpatient services out of St Peter’s Hospital, as described on page 16, would have left the birthing unit isolated as the only 24-hour service on the site. Staff and service leaders told us they were concerned about safety out of hours. The WJC birthing unit is on a site with other 24-hour services. It is a modern purpose-built suite with better facilities that allow us to care for more families wanting to give birth in a freestanding midwife-led birthing unit.
Since moving the service to the WJC birthing unit, the average number of births has increased to 9 each month.
Other patient services at St Peter’s Hospital, Maldon
We fund a range of other services that operate out of St Peter’s Hospital that provide around 300 patient appointments on each clinic day. That’s more than 80,000 appointments each year. These appointments include:
- 39,000 outpatient appointments
- 37,000 blood tests
- 8,500 X-ray appointments
- 700 ultrasound examinations
The 2019 NHS Long Term Plan sets out the need to transform the approach to these services. NHS England expects all health and care systems to reduce follow up appointments by 25%, which for the St Peter’s Hospital services is significant.
The age, condition and suitability of St Peter’s Hospital had caused plans to be developed to provide purpose-built replacement local facilities. It is clear that these new facilities will not be built for some years. It is equally clear that to keep St Peter’s Hospital open and operating safely, we would have to fix all the problems with the buildings, and bring it up to standard for the delivery of NHS services. Fixing all the problems would cost an estimated £18.7m. That is more money than is available. Bringing the hospital up to modern standards would cost more again.
Alternative short-term solutions are needed if residents of Maldon and surrounding districts are to continue to have local access to these services pending decisions on the development of alternative health facilities for local people. Patients from other districts could access appointments nearer to them.
The condition of St Peter’s Hospital, Maldon
St Peter’s Hospital, owned by the Mid and South Essex NHS Foundation Trust, is an old facility in central Maldon. Built 150 years ago, it originally served as a Victorian Poor Law Workhouse. The structures, including additional buildings from the 1940s and 1960s, are costly to maintain due to their age. The site includes Cherry Trees Therapy Centre, a mental health facility owned by Essex Partnership University NHS Foundation Trust.
Lots of repair work is still needed. And lots more work is needed to bring the hospital up to required standards. Damp is visible all through the hospital, rain leaks through the roof into working areas, and asbestos in the buildings is managed with annual inspections. A recent survey showed that there are signs of defects in 76% of the total internal area. Half of those defects (52%) are high risk.
There are concerns about the safety and the suitability of the building as a location for providing clinical care as it does not meet the required standards. Because of this, inpatient services have been temporarily moved to other hospitals, and through this consultation we are looking into the possibility of moving all the other patient services at St Peter’s Hospital to other premises, mostly in and around Maldon. To keep St Peter’s Hospital open, we would have to fix all the problems and bring it up to standard for the delivery of NHS services. An independent assessment estimates it would cost £18.7m to fix all the problems. That is more money than is available and there would still be more work to do to bring the building up to standard.
Our first priority is the safety and welfare of patients and staff. Mid and South Essex NHS Foundation Trust has carefully assessed the situation at St Peter’s Hospital. Outpatient and clinic appointments only happen in the areas of the hospital that are safe.
76% of the total internal area shows signs of defects
52% of those defects are high risk
An independent assessment estimates it would cost £18.7m to fix all the problems. That is more money than is available and there would still be more work to do to bring the building up to modern standards.
How we developed our proposals
We used a range of national guidance, local data, our senior doctors’ and nurses’ clinical experience, and advice from others to work out how many patients would benefit from being cared for in a bed in one of our community hospitals.
We started with stroke rehabilitation and intermediate care inpatient services in community hospitals. Some of these services are normally based at St Peter’s Hospital, Maldon. In our review, we looked at how suitable the buildings at St Peter’s Hospital are for those services and how the services there rely on each other.
In this process, we identified a need to look at the future of our freestanding midwifeled birthing unit, and the future of all other services at St Peter’s Hospital, Maldon. In each case, a working group made up of doctors, nurses, other health and care staff, and service leaders worked together, taking into account the feedback given by patients, staff and residents.
After considering financial, strategic and quality criteria, and the five tests of service change required by the Government and NHS England, we arrived at the proposals we present to you in this consultation.
The five tests of service change set out by NHS England
- Strong public and patient engagement.
- Consistency with current and prospective need for patient choice.
- Clear, clinical evidence base.
- Support for proposals from clinical commissioners.
- Careful consideration of the number of hospital beds needed
Stroke rehabilitation and intermediate care inpatient services in community hospitals
Our taskforce of local doctors, nurses, and other service leaders looked at the performance of the services we offer normally and identified where we need to improve. We looked at predicted changes in the population and worked out how many patients we can expect. And we looked at information from other areas to see what we can learn from them. We took into account that: The number of people in the target population is expected to increase by 8% in the next five years. 95% of the community hospital beds we provide will be used at any one time. Stroke rehabilitation should be a dedicated service provided in one place, or at most two places. We calculated that in our community hospitals we need: between 77 and 87 intermediate care beds. between 48 and 50 stroke rehabilitation beds.
We looked at the facilities we have available to us and developed a list of 13 different ways we could organise these services. None of these ideas included continuing to use St Peter’s Hospital in Maldon, because we considered its poor state of repair unsuitable for inpatients. Our list of 13 possible ways of organising these services was cut down to four by a group of local doctors, nurses and other health and care staff. Of those four, there are two that: allow us to improve care by working in the best clinical ways, and give us the capacity in our community hospitals that our estimates tell us we need. In this consultation we are presenting those two as proposals on page 20 – 30.
Freestanding midwife-led birthing unit
Our working group of doctors, midwives and other service leaders started with a list of ideas for the future of the freestanding midwife-led birthing unit provided at St Peter’s Hospital, Maldon. The group noted that to keep the service at St Peter’s Hospital, there would need to be other 24 hour services at the hospital; and removed the idea not to have a freestanding midwife-led birthing unit, because that would limit birthing choices for mid and south Essex residents. That left seven potential ideas: three variations involving combining the service with the maternity service in Chelmsford, three variations using the WJC birthing unit facility at Braintree Community Hospital, and an idea to put the service in a new primary care hub in Maldon.
We ruled out the variations at Broomfield Hospital because the service there is already at capacity. Ideas that included putting the service at a new primary care hub in Maldon were ruled out because it would take too long to put in place and would cost more than the money we have available. And we recognised that the WJC birthing unit isn’t big enough to accommodate the outpatient maternity services as well as the birthing services. That left us with one viable option that we present on page 27 of this consultation document.
Other patient services at St Peter’s Hospital
Our work to understand the condition of the buildings at St Peter’s Hospital in Maldon made us think about how suitable they are for any patient services. We identified advantages to moving the other outpatient services out of St Peter’s Hospital and started to think about where we could move them to. We have started to identify some potential new homes for these services in and around Maldon. We are committed to involving patients and local people as we explore alternatives.
It’s harder to find suitable accommodation for services that use specialist equipment, like X-ray. We might need to look a bit further away for those. And some services rely on other services being in the same place as other services, for example, orthopaedics and rheumatology need to be in the same place as radiology. In those cases we might need to ask patients to travel outside Maldon. Work to identify suitable alternative accommodation continues.
If we decide that services we are responsible for won’t be provided at St Peter’s Hospital, we know it’s likely that Mid and South Essex NHS Foundation Trust and Essex Partnership University NHS Foundation Trust, the owners of St Peter’s Hospital and the Cherry Trees Therapy Centre, will decide to close the hospital permanently. So in this consultation we’re asking for your views on the idea of moving all services out of St Peter’s Hospital. We’d like to know what you think of the idea and how you think it would impact you and the people you know and care for.
Consultation proposals
The proposals that we are describing in this document are just that: proposals. We are asking local people to share their thoughts before we decide what to do. We will consider your responses carefully and take them into account when we’re making decisions about these proposals.
Proposals for Intermediate care and stroke rehabilitation inpatient services
Normal operational position
We pay the following organisations to provide the services needed to run intermediate care and stroke rehabilitation beds in mid and south Essex:
- Mid and South Essex NHS Foundation Trust,
- Essex Partnership NHS Foundation Trust,
- Provide Community Interest Company,
- North East London NHS Foundation Trust.
The contractual arrangements we have in place provide:
- Stroke rehabilitation community hospital beds at:
- St Peter’s Hospital, Maldon (16 beds), and
- Rochford, Cumberlege Intermediate Care Centre (8 beds)
- Intermediate care community hospital beds at:
- Billericay – Mountnessing Court (22 beds)
- Brentwood, Brentwood Community Hospital (25 beds)
- Grays, Thurrock Community Hospital (24 beds)
- Halstead, Halstead Hospital (20 beds), and
- Rochford, Cumberlege Intermediate Care Centre (14 beds)
Temporary operational position (winter 2023/24)
In August 2023, we approved temporary changes to these services to make sure they can run effectively through the winter period. This meant in October 2023:
- closing 16 stroke beds at St Peter’s Hospital, Maldon
- opening 25 stroke beds at Brentwood Community Hospital, and
- converting 6 intermediate care beds in Rochford to accommodate stroke rehabilitation patients.
The temporary operational arrangements we have in place provide:
- Stroke rehabilitation community hospital beds at:
- Brentwood, Brentwood Community Hospital (25 beds), and
- Rochford, Cumberlege Intermediate Care Centre (14 beds)
- Intermediate care community hospital beds at:
- Billericay – Mountnessing Court (22 beds)
- Brentwood, Brentwood Community Hospital (25 beds)
- Grays, Thurrock Community Hospital (24 beds)
- Halstead, Halstead Hospital (20 beds), and
- Rochford, Cumberlege Intermediate Care Centre (8 beds)
These actions: increased from 24 to 39 the number of stroke rehabilitation beds available in our community hospitals. Still around 10 beds short of how many we need, and reduced by 5 the number of intermediate care beds available in our community hospitals. That’s still around 10 beds more than the number we’ve calculated we need.
Our proposals
We are consulting on two options for arranging intermediate care beds and stroke rehabilitation beds at our community hospitals. These are in addition to the independent living and rehabilitation support we and our local councils already provide to patients at home, in residential care places, and in community clinics.
Option A would provide 138 beds:
- Stroke rehabilitation community hospital beds at:
- Brentwood, Brentwood Community Hospital (50 beds)
- Intermediate care community hospital beds at:
- Billericay – Mountnessing Court (22 beds)
- Grays, Thurrock Community Hospital (24 beds)
- Halstead, Halstead Hospital (20 beds), and
- Rochford, Cumberlege Intermediate Care Centre (22 beds)
Option B would provide 138 beds:
- Stroke rehabilitation community hospital beds at:
- Brentwood, Brentwood Community Hospital (25 beds), and
- Rochford, Cumberlege Intermediate Care Centre (22 beds)
- Intermediate care community hospital beds at:
- Billericay – Mountnessing Court (22 beds)
- Brentwood, Brentwood Community Hospital (25 beds)
- Grays, Thurrock Community Hospital (24 beds), and
- Halstead, Halstead Hospital (20 beds)
Impacts for both options
Specialised care offers more options to help more patients recover and regain independence.
- Fewer long stays in acute hospitals, reducing risks of hospital-acquired infections. ► People living in Braintree district and Maldon district will likely have to travel further for inpatient stroke rehabilitation support.
- Stroke rehabilitation inpatient care will no longer be provided at St Peter’s Hospital, Maldon
- Carers and visitors often travel more regularly than patients, so increased or reduced travel is likely to impact them more. This could be particularly impactful for people who have mobility difficulties or disabilities, and people who rely on public transport.
- Stroke patients will receive care in modern, better equipped facilities.
- The need for community hospital beds might go down as processes are improved and more people receive intermediate care in other settings, including at home.
- Specialist centres are considered more attractive to potential new staff.
- Providing dedicated stroke rehabilitation services will ensure expertise is easily available, which should mean more patients regain more of their independence.
- The other facilities offering intermediate care beds would be the Mayfield Unit at Thurrock Community Hospital with 24 beds, Mountnessing Court in Billericay with 22 beds, and Halstead Hospital in the north of mid and south Essex with 20 beds. These numbers would not be affected by the proposals.
Option A
Option A would provide a combined total of 138 beds:
- 50 stroke rehabilitation community hospital beds at:
- Brentwood, Brentwood Community Hospital (50 beds)
- Brentwood, Brentwood Community Hospital (50 beds)
- 88 intermediate care community hospital beds at:
- Billericay – Mountnessing Court (22 beds)
- Grays, Thurrock Community Hospital (24 beds)
- Halstead, Halstead Hospital (20 beds), and
- Rochford, Cumberlege Intermediate Care Centre (22 beds)
This option would mean
- A single, 50-bed Stroke rehabilitation unit at Brentwood Community Hospital, Brentwood.
- 22 intermediate care beds at Cumberlege Intermediate Care Centre, Rochford.
- A single, 50-bed Stroke rehabilitation unit at Brentwood Community Hospital, Brentwood. 22 intermediate care beds at Cumberlege Intermediate Care Centre, Rochford.
Option A: predicted impacts
- People from Brentwood, Basildon, Thurrock and parts of Chelmsford will likely have to travel less far for inpatient stroke rehabilitation support. Carers and visitors often travel more regularly than patients, so reduced travel from these areas is likely to impact them more.
- People from Castle Point, Maldon, Rochford and Southend-on-Sea will likely have to travel further for inpatient stroke rehabilitation support.
- Three less intermediate care beds would be available than in Option B.
- Three more stroke rehabilitation beds would be available than in Option B.
- Expands the options in the area for people who need some types of neuro-rehabilitation, reducing the need for some patients, carers, and relatives to travel out of the area for care.
- Specialist centres are considered more appealing to a specialist workforce.
- There would be no intermediate care beds at Brentwood (currently 25), the nearest would be at Mountnessing Court in nearby Billericay (22 beds)
- This option is forecast to cost £0.2 million more than current costs over the next 11 years.
Option B
Option B would provide a total of 138 beds:
- 47 stroke rehabilitation community hospital beds at:
- Brentwood, Brentwood Community Hospital (25 beds), and
- Rochford, Cumberlege Intermediate Care Centre (22 beds)
- 91 intermediate care community hospital beds at:
- Billericay – Mountnessing Court (22 beds)
- Brentwood, Brentwood Community Hospital (25 beds)
- Grays, Thurrock Community Hospital (24 beds), and
- Halstead, Halstead Hospital (20 beds)
This option would mean
- A 25-bed stroke rehabilitation unit at Brentwood Community Hospital, Brentwood
- 25 intermediate care beds at Brentwood Community Hospital, Brentwood.
- A 22-bed stroke rehabilitation unit at Cumberlege Intermediate Care Centre, Rochford
- Permanently closing the stroke rehabilitation ward at St Peter’s Hospital, Maldon.
Option B: predicted impacts
- The Cumberlege Intermediate Care Centre (CICC) in Rochford would have 22 stroke rehabilitation beds accessible to people living in south east Essex, 14 more than now.
- Two smaller stroke rehabilitation units would give people living in the west and south east of the area good access and offer them a choice.
- People from Castle Point, Maldon, Rochford and Southend-on-Sea will likely have to travel further for inpatient intermediate care services. Carers and visitors often travel more regularly than patients, so increased travel is likely to impact them more. This could be particularly impactful for people who have mobility difficulties or disabilities, and people who rely on public transport.
- Three more intermediate care beds would be available than in Option A.
- Three less stroke rehabilitation beds would be available than in Option A.
- The CICC in Rochford would need some bathroom alterations if it were to be used solely for stroke rehabilitation.
- It would not be possible for this option to accommodate neuro-rehabilitation beds.
- This option is forecast to cost £14.1 million less than current costs over the next 11 years.
Other ideas we considered
An idea to create a central intermediate care centre and have beds on up to five other sites was dismissed. The idea would need lots of funding and time. There is no sign that the funding would be available, and the changes need to be made soon. This means using existing sites that meet required standards is the only practical approach. We looked at the buildings we have and developed a list of 13 different ways we could organise these services. None of these ideas included continuing to use St Peter’s Hospital, Maldon, because we considered its poor state of repair unsuitable for inpatients. Our list of 13 possible ways of organising these services was cut down to four by a group of local doctors, nurses and other health and care staff. We discarded two of those four ideas:
Idea 1 would provide a combined total of 138 beds:
- 39 stroke rehabilitation community hospital beds at:
- Brentwood, Brentwood Community Hospital (25 beds), and
- Rochford, Cumberlege Intermediate Care Centre (14 beds)
- 99 intermediate care community hospital beds at:
- Billericay – Mountnessing Court (22 beds)
- Brentwood, Brentwood Community Hospital (25 beds)
- Grays, Thurrock Community Hospital (24 beds)
- Halstead, Halstead Hospital (20 beds), and
- Rochford, Cumberlege Intermediate Care Centre (8 beds)
Idea 2 would provide a combined total of 116 beds:
- 39 stroke rehabilitation community hospital beds at:
- Brentwood, Brentwood Community Hospital (25 beds), and
- Rochford, Cumberlege Intermediate Care Centre (14 beds)
- 77 intermediate care community hospital beds at:
- Billericay – Mountnessing Court (22 beds)
- Brentwood, Brentwood Community Hospital (25 beds)
- Grays, Thurrock Community Hospital (24 beds)
- Halstead, Halstead Hospital (20 beds), and
- Rochford, Cumberlege Intermediate Care Centre (8 beds)
Idea 1 is the model that has been put in place on a temporary basis for winter 2023-24. Ideas 1 and 2 do not achieve our target number of stroke rehabilitation beds. Both include providing support for a mix of stroke rehabilitation and intermediate care patients at the Cumberlege Intermediate Care Centre in Rochford. Mixed units cost more than providing one type of care at each location. And taking into account that dedicated units mean more travel for some relatives and carers, specialist doctors and nurses say dedicated units are better for patients’ recovery. For these reasons, ideas 1 and 2 are not presented as proposals in this consultation. *In the pre-consultation business case (PCBC), Idea 1 appears as option 4, and Idea 2 appears as option 5.
Proposal for freestanding midwife-led birthing Unit
Our proposal on future arrangements for freestanding midwife-led birthing services
Normal operational position
We buy freestanding midwife-led birthing services from Mid and South Essex NHS Foundation Trust. The contractual arrangements we have in place provide these services at St Peter’s Hospital, Maldon. In the past few years, the birthing unit at St Peter’s Hospital was sometimes closed because not enough staff were available.
Temporary operational position (winter 2023/24)
In August 2023, we approved temporary changes that moved stroke rehabilitation services from St Peter’s Hospital to Brentwood Community Hospital, to make sure they can run safely and effectively through the winter period. That would have left the birthing unit isolated. Staff and service leaders told us they were concerned about safety out of hours, and the service has the same issues with the poor condition of the buildings at St Peter’s Hospital impacting the quality of care we can provide there. So we decided to move the birthing unit to the WJC Birthing unit in St Michael’s Health Centre at Braintree Community Hospital where there is a larger, modern purpose-built birthing suite and other 24-hour services. This change did not affect antenatal and postnatal outpatient clinics, which still take place at St Peter’s Hospital in Maldon.
Our proposal
We are consulting on one option for the location of a freestanding midwife-led birthing unit in our area.
Option: A freestanding midwife-led birthing unit to be based at the WJC Birthing unit in St Michael’s Health Centre at Braintree Community Hospital.
This option would mean:
- Eligible people would have the choice to travel to Braintree to give birth, supported by
their midwives.
- Where there are complications that need hospital support, patients would transfer to Broomfield Hospital, Chelmsford.
Predicted impacts
- Better, more modern facilities which are consistently open and available.
- Easier travel for many in the mid and south Essex area.
- An increase in the number of births in our freestanding midwife-led service.
- People from south and east Essex would travel further for this service, incurring additional costs. This impact could be greater for people with disabilities, people living in poorer areas, and people who rely on others for transport.
- Options to work in low-risk community settings broaden our recruitment offer to potential staff.
If there are complications during birth that need hospital support, the transfer time to Broomfield Hospital from the WJC Birthing Unit is 16 minutes, compared to 28 minutes
from St Peter’s Hospital in Maldon.
- A more reliable community option for low-risk births will likely reduce pressure at other maternity units in the area and offer people more consistent choice of where to give birth.
- We forecast that the costs of running the freestanding midwife-led birthing unit in Braintree will be the same as they are for running it in Maldon.
Other ideas we considered
We looked at seven possibilities. We eliminated an idea to have no freestanding midwife-led birthing unit because that would limit birthing choice options in our area. We eliminated an idea to create an inpatient and outpatient maternity service at a primary care hub in Maldon because of the limits on funding available and the time it would take. We eliminated ideas based in Chelmsford, because Broomfield Hospital maternity unit is already at capacity. That left a shortlist of three ideas, all based around the WJC Birthing unit in St Michael’s Health Centre at Braintree Community Hospital.
2a Move St Peter’s Hospital inpatient and outpatient maternity services to WJC
2b Move St Peter’s Hospital inpatient maternity services to WJC and re-provide outpatient services in Maldon
2c Move St Peter’s Hospital inpatient maternity services to WJC and re-provide outpatient services in co-location with Maldon primary care development
We eliminated the idea (2a) to move St Peter’s Hospital inpatient and outpatient services to WJC, because there would not be enough room for all the outpatient services at WJC. And we eliminated idea 2c, because limited available funding means a new primary care facility in Maldon is unlikely to be developed quickly.
Your views on the future of other patient services at St Peter’s Hospital, Maldon
The age, condition and suitability of St Peter’s Hospital means we are thinking about the need to provide alternative accommodation for the other services we provide in Maldon.
We fund a range of other services that operate out of St Peter’s Hospital that provide around:
- 300 patient appointments on each clinic day
- 80,000+ appointments each year.
The services provided at St Peter’s:
- Abdominal aortic aneurysm (AAA) – screening for swelling in the main blood vessel that runs from your heart down through your body
- Assessment and Rehab Unit (incl. COPD)
- Audiology
- Bladder and Bowel
- Cardiology – heart conditions
- Catheter Clinic
- Children’s continence
- Communication station initial assessments
- Day Therapy
- Dermatology – skin conditions
- Diabetes
- Dietetics – food and nutrition
- District Nursing
- Endocrinology – conditions of glands and hormones
- Ears, nose and throat
- Gastroenterology – stomach and intestines
- General Medicine
- Long Covid
- Maternity hub – including obs and gynae, paediatrics, neonatal and midwife OPs, scanning and classes
- Mental health services provided in
- Cherry Trees Therapy Centre
- Nephrology – kidney conditions
- Neurology – conditions affecting the nervous system
- Ophthalmology – eye conditions
- Optometry – eye examinations
- Orthopaedics – bone, joint and cartilage related conditions
- Orthoptics – eye movement disorders and vision development
- Out-of-hours GP
- Oxygen
- Parkinson’s
- Phlebotomy – blood tests
- Physiotherapy
- Podiatry
- Pulmonary Rehabilitation – helping people with lung conditions breathe better
- Radiology and Ultrasound – x-ray and other diagnostic services
- Rheumatology – conditions affecting the joints and surrounding tissues
- Speech and Language Therapy
There are concerns about the safety and the suitability of the building as a location for providing clinical care in the future as it does not meet the required standards. An independent assessment estimates it would cost £18.7 million to do the building work to fix all the problems at St Peter’s Hospital. That amount of money isn’t available, so this isn’t a viable option for us. If the money was available, we would still have to move services to keep our patients and staff safe. We have also looked at the possibility of demolishing the Villas and ‘C’ Block at the back of St Peter’s Hospital to put up temporary accommodation for patient services there. There would be a considerable cost to do that work and we know that NHS temporary buildings can, unintentionally, become permanent. For these reasons, this isn’t a viable option for us either.
The solution we are exploring is to find other suitable accommodation for these services in and around Maldon including buildings that aren’t used at the moment. We are unlikely to find a single place where all these services can go together, which means different services would likely be in different buildings. We would aim to keep services that rely on each other together. For example, orthopaedics and rheumatology would have to be in the same place as radiology, so patients don’t have to go somewhere else for X-ray and other diagnostic services. Patients from other districts could access appointments nearer to them.
The annual costs of using different accommodation are expected to be the same as at St Peter’s Hospital. The cost of moving and adapting other venues to be suitable for use is estimated at £3 million.
We are committed to working with service users and local people to develop our plans and make sure key services remain local. We have started to assess some of the buildings we think might be suitable as alternative accommodation and will continue that work to make sure we fully understand all the options.
We’re hopeful of finding appropriate accommodation for all these services in and around Maldon. Orthopaedics and rheumatology need to be where radiology and ultrasound are, so we might need to look outside Maldon District for somewhere that can be a home to these services. One possibility we’re looking at is basing these services at Braintree Community Hospital, 16 miles from Maldon. If we make a decision that none of the health services we are responsible for will be provided at St Peter’s Hospital, it is likely that Mid and South Essex NHS Foundation Trust, and Essex Partnership University NHS Foundation Trust, as the site owners, would decide to close St Peter’s Hospital permanently. For those reasons, we would like to hear your views on what we should take into account before we make the decision to move all services from the site.
Staffing, equality and health inequalities issues
Staffing issues
We often find it difficult to recruit trained nurses, therapists and other healthcare professionals to work in our services. Many other areas in England have the same difficulties. There aren’t enough trained staff to fill all the jobs, so there is competition from hospitals in other areas for people with the right skills and qualifications.
Community beds have proven difficult to staff. When we can’t recruit enough staff, we have to use agency staff and bank staff. That reduces continuity for our patients at the same time as increasing costs.
The ways our staff work were disrupted during the COVID-19 pandemic when we had to move services to keep people as safe as we could. They have been disrupted again as we’ve had to make temporary changes to services, like closing the birthing unit at St Peter’s Hospital, Maldon from time to time, and reorganising stroke rehabilitation beds and intermediate care beds to make best use of our people and facilities this winter. This creates uncertainty for staff and has meant some jobs have been advertised on a fixed-term basis, which isn’t as attractive as a permanent job.
We are close to London. NHS staff in London are paid more than staff in the other areas of the country, and qualified people in our area can easily travel into London for work. The jobs have in our area must be professionally and personally attractive, if we are to compete. Stable service arrangements in accommodation that offers good working conditions and is clinically suitable will be more attractive to potential recruits than how things are at the moment.
Equality and health inequalities issues
Health inequalities describes the gap in accessing services, receiving appropriate treatment, and experiencing good health outcomes, between groups of people.
People experiencing health inequalities are often people with protected characteristics (for example age, race, sexuality). People can also be disadvantaged by other factors such as where they live, financial circumstances, mental health, refugee status, homelessness or caring responsibilities. It’s important to consider the impact of proposals on people whose circumstances could already be at a disadvantage when needing health or care services.
The mid and south Essex area has 120,840 people in the most deprived 20% of England. This equates to approximately 10% of the population here.
Some of the groups of people identified as being impacted by health inequalities are:
Carers: Informal caring can place people under stress and increase certain health risks. Carers can experience health inequalities, especially people who face additional barriers to accessing care, for example where English is not a first language.
In mid and south Essex 115,776 people are providing unpaid care. This number could be higher as many family members do not consider themselves to be carers. Southend and Basildon have the highest volume of unpaid carers.
Homelessness: Statutory homelessness is defined as households living in temporary accommodation provided under homeless legislation.
People experiencing homelessness are at a higher risk of long-term conditions and mental ill health. Being homeless also increases risk of delayed discharge from hospital, and problems related to homelessness can lead to repeated hospital admissions.
Records showed around 5000 households in statutory homelessness in mid and south Essex in 2019/20. The largest number of those in Thurrock, followed by Southend.
This number does not include people who are street homeless, sofa-surfing or otherwise unknown to statutory systems.
Mental health: People with long-term conditions have significantly raised rates of depression, anxiety and other mental health problems. Evidence suggests that many of these people receive poorer quality care than those with a single condition.
As of 2020/21, there were 10,236 people in mid and south Essex with a diagnosis of schizophrenia, bipolar affective disorder and other psychoses. An Adult Psychiatric Morbidity Survey conducted in 2016 identified over 130,000 people with mental health disorders in our area. Basildon had the highest volume of people self-reporting.
Substance misuse: Patients with substance use disorder diagnoses, specifically those with drug use-related diagnoses, have higher rates of recurring hospital admissions than those without substance use disorder diagnoses. According to the 2018 Health Survey for England, 30,962 people in our area are at higher risk of alcohol-related health problems, and 23,370 are dependent on drugs according to the Adult Psychiatric Morbidity Survey, 2016 release. Basildon has the highest volume of both, followed by Southend and Thurrock.
Gypsy, Roma and Traveller communities: Compared with the general population, people from Gypsy, Roma, and Traveller communities are more likely to experience poor health. This includes lower life expectancy, high infant mortality rates, high maternal mortality rates, higher prevalence of anxiety and depression, and long-term conditions.
There is currently a lack of data to ascertain whether Gypsy, Roma and Traveller communities will be disproportionately affected by the proposals.
Refugees and asylum seekers: Refugees and asylum seekers can have complex health needs. These may be influenced by experiences prior to leaving their home country, during transit or after arrival in the UK. People might arrive in the UK with chronic conditions, such as diabetes or hypertension. This is often exacerbated by long periods without access to regular care.
Involving people affected by health inequalities: It is important to try to engage with local communities to understand more about barriers and how the proposed changes to services could improve patient experience. It is also important that information is designed in accessible formats. Our consultation plan includes mechanisms for reaching out to people more likely to experience health inequalities who could be adversely impacted by the proposals. For example, by connecting with community groups, tenants’ associations, specialist patient groups and using targeted communications.
Have your say
The consultation runs for 8 weeks, from 25 January 2024 to 11 April 2024 and there are many ways in which you can find out more and take part.
This public consultation aims to give local people and communities the opportunity to share their views and ideas on:
- our proposals for potential changes to the locations where we provide some of our inpatient services for community hospital intermediate care and stroke rehabilitation, and freestanding midwife-led birthing services; and
- the possibility of moving all other patient services at St Peter’s Hospital, Maldon to other locations, mostly in and around Maldon.
There are several ways to have your say. You can fill in our consultation survey which is available on our website. Paper copies of the survey are available at libraries and other public venues.
You can attend a consultation event:
| Date | Time | Venue |
|---|---|---|
| 5th February | 6pm – 7.30pm | The Beehive Centre, Thurrock |
| 7th February | 6pm – 7.30pm | Marconi Room, Chelmsford Civic Centre |
| 12th February | 2pm – 3.30pm | Online maternity event |
| 13th February | 2pm – 3.30pm | Online stroke rehabilitation event |
| 15th February | 10.30am – 12pm | Online intermediate care beds event |
| 15th January | 5pm – 6.30pm | The Forum, Southend |
| 26th February | 2pm – 3.30pm | Online patient services at St Peter’s Hospital event |
| 28th February | 6pm – 7.30pm | Online event covering all changes |
| 6th March | 4pm – 5.30pm | Ormiston Rivers Academy, Burnham on Crouch |
| 6th March | 6.30pm – 8.30pm | Ormiston Rivers Academy, Burnham on Crouch |
Public consultation hearing
We are holding a public consultation hearing at: Maldon Town Hall on Tuesday 19th March. You can: attend as an observer, watch online, or give evidence to the panel. If you would like to give evidence, please register via our website, or contact us by Thursday 7th March. All dates, time and locations are correct at the time of print, and you can register to attend an event via our website.
Please register in advance for events so we can ensure they are appropriately staffed in order to get the very best out of them. The consultation website has the most up to date information. NHS staff will have the opportunity to attend dedicated staff events.
Join the conversation on Virtual Views, the Mid and South Essex online engagement hub.
If you need any help, contact us.
Contact us
- Email: [email protected]
- X (formally Twitter)
- Telephone: 01268 594350
- Write to us: FAO: Community Capacity Consultation, NHS Mid and South Essex ICB, PO Box 6483, Basildon, SS14 0UG
What happens next
Mid and South Essex Integrated CareBoard (ICB) welcomes your responses. All responses and feedback will be analysed and reported by an independent organisation and we will publish their report ahead of the meetings that consider the proposals. The ICB plans to consider the proposals in the context of all the feedback received from the public, organisations and staff over the summer of 2024.
Any decisions the ICB makes about the future of inpatient stroke rehabilitation and intermediate care beds and the freestanding midwife-led birthing unit would then be implemented.
There would be work to do to prepare for the changes to inpatient stroke rehabilitation and intermediate care beds. The earliest we could expect the changes to be made is October 2024.
The proposal for permanent changes to the location of the freestanding midwife-led birthing unit are the same as the current temporary arrangements. So it is likely only administrative changes would be needed in this case.
If the ICB decides that it no longer wants to commission services at St Peter’s Hospital, a series of other assessments and decisions would follow about where each service would be relocated to. Then it is likely services would move on a planned basis over a period of time as alternative accommodation is made ready. Patients and local people would have the opportunity to be involved and would be kept in touch throughout. It is likely that the boards of Mid and South Essex NHS Foundation Trust and Essex Partnership University NHS Foundation Trust will consider the future of St Peter’s Hospital and Cherry Trees Therapy Centre. If they decide to close the hospital permanently, the site would be sold and the money from the sale used for NHS services in the area.