Trying for a baby
The decision to start a family is an important step that many couples make together. When couples start trying to conceive but are finding it hard, it can be both disheartening and stressful, but you are not alone. As many as 1 in 7 heterosexual couples will struggle to conceive naturally; that’s as many as 3.5 million people in the UK.
Conceiving naturally can take time. You and your partner should aim to have regular sex every two to three days without any form of contraception. It can sometimes take a while for some types of contraception to stop working which may affect your ability to get pregnant initially.
Conceiving is a very natural but also very complicated part of life. Sometimes it can feel like you are in the dark about what is going on which can be very frustrating, but if you have been trying less than a year and are aged under 36, then there may be no need to seek help. If you have been trying for over a year without success, then you can speak to your GP about what may be going on and also find out ways that might help boost your chances of getting pregnant.
Seeing your GP
Your GP should be the first health professional you see to discuss why you are finding it difficult to conceive. Both you and your partner should book an appointment so that your GP can start investigations to find out why you may be struggling to get pregnant.
During the appointment, your GP will ask you a series of questions about your medical and sexual history and also your lifestyle. They may also conduct a physical examination of your pelvic area if you’re a woman or your testicles and penis if a man. Some of the questions and the physical examination may make you feel uncomfortable, but remember your GP is trying to help and needs to ask questions and conduct examinations so that they can narrow down potential causes.
After asking questions about your fertility, you will then be asked to provide a number of samples which can then be tested.
Female investigations include:
- Blood test to check hormone levels which can reveal details about your egg production;
- Cervical screening to check for abnormal cells which can have an effect on pregnancy and birth;
- Ultrasound scan to check the womb for conditions that can prevent pregnancy;
- Chlamydia test to test for chlamydia which can affect fertility.
Male investigations include:
- Semen Analysis so that the health of your sperm can be determined;
- Chlamydia test due to its effect on fertility.
After your appointment, you can continue to try and conceive naturally. Your GP will give you some recommendations based on your lifestyle answers which could help boost your chance on conceiving. These may include dietary changes or quitting smoking. You can find out more about lifestyle changes that can boost pregnancy on the NHS website:
NHS pregnancy questions NHS advice for optimising male fertility Example patient fertility pathwayYour GP may refer you to a consultant within secondary care (hospital) for further investigations.
What happens when you are referred to the hospital?
Further tests may be completed to investigate what may be preventing you and your partner from becoming pregnant. Some of these will be similar to the ones carried out by your GP, some others may be new to you. The tests may include:
- Physical examination / medical history: you and your partner will both be asked about your medical history. Your height and weight will be recorded and the doctor may ask to examine you.
- Blood tests: You or your partner may be asked to provide a blood sample to run some checks such on your hormone levels.
- Chlamydia test or chlamydia swab
- Repeat semen analysis if necessary
- An ultrasound will be requested
After the first appointment, your consultant will discuss the findings of your tests and what is the best way forward. This could include a number of procedures which can help boost you chances of getting pregnant. This includes Ovulation Induction which is a fertility treatment for women that encourages the production and release of eggs.
Depending on the results of your tests, some further investigations may be needed to see why you are struggling to conceive. You may be referred to one of the commissioned Assisted Conception Units (ACU) for In Vitro Fertilisation (IVF) or Intacytoplasmic Sperm Injection (ICSI), if you meet the eligibility criteria.
View our Tertiary Fertility Services policy for eligibility criteriaWhat is IVF?
In vitro fertilisation (IVF) is one of several techniques available to help people with fertility problems have a baby. During IVF, an egg is removed from the woman’s ovaries and fertilised with sperm in a laboratory. The fertilised egg, called an embryo, is then returned to the woman’s womb to grow and develop.
Find out more about IVFWhat happens if you are referred for IVF treatment?
Following your consultation within secondary care, your consultant or fertility nurse will complete a prior approval form which will be sent to the Funding Team who process applications for residents in mid and south Essex. A decision will be made based on the clinical information provided which evidences that the couple meet the criteria for NHS funded treatment within the mid and south Essex area.
Your consultant or fertility nurse will notify you of the decision made. If funding is declined, an explanation will be provided to the Trust to enable them to feedback to the couple. Please note that either your GP or another clinical professional can appeal the decision to decline funding, however this will only be considered on receipt of additional clinical evidence. Patients who do not meet the full criteria will not be offered NHS tertiary fertility treatment.
If your funding is approved, you will then be able to attend an Assisted Conception Units (ACU) to discuss fertility treatment. You can choose from the following clinics:
- Bourn Hall Clinic, 25 London Road, Wickford, SS12 0AW
- CARE Fertility London, Park Lorne, 111 Park Road, London NW8 7JL
- Create Fertility – St Georges House, 3-5 Pepys Road, West Wimbledon SW20 8NJ
- Create Fertility – St Paul’s, 150 Cheapside, London, EC2V 6ET
- Cambridge Hospital, Women’s and Children’s Services, Cambridge University Hospitals, NHS Foundation Trust, Rosie Hospital, Cambridge Biomedical Campus
- Guy’s & St Thomas, NHS Foundation Trust, 11th floor, Tower Wing, Great Maze Pond, London SE1 9RT
- Herts and Essex Fertility Centre, Bishops College, Churchgate, Chestnut, Waltham Cross, EN8 9XP
- IVI London Wimpole, 83 Wimpole Street, London, W1G 9RQ
(The clinics that provide IVF and ICSI are subject to change.)
Same-sex female couples
For same-sex female couples where one of you is trying to become pregnant, the first treatment option is self-funded intrauterine insemination (IUI). Please refer to our Tertiary Fertility Policy for further information.)
Additional information about specialist fertility treatments:
IVF (In Vitro Fertilisation) and ICSI (Intracytoplasmic Sperm Injection) are both a form of treatment that involves collecting some eggs from a female partner and fertilising them with sperm in the lab. Once the eggs have been fertilised, one or two embryos will be placed back in to the womb. The two treatments differ in the number of sperm used. with IVF, the egg is added to a solution containing a large number of sperm. With ICSI, one sperm is injected directly into the egg. ICSI is used if sperm is unlikely to fertilise an egg naturally.
To collect the eggs that are to be used in either IVF or ICSI treatment, medication will be given to the partner who is trying to become pregnant. This medication will stop the natural cycle of egg production. You will also receive daily injections that will boost the number of eggs that mature. A short procedure will then take place to collect a number of eggs which will be fertilised using a sperm sample from either your partner or a donor. One or two eggs are then placed back into the uterus.
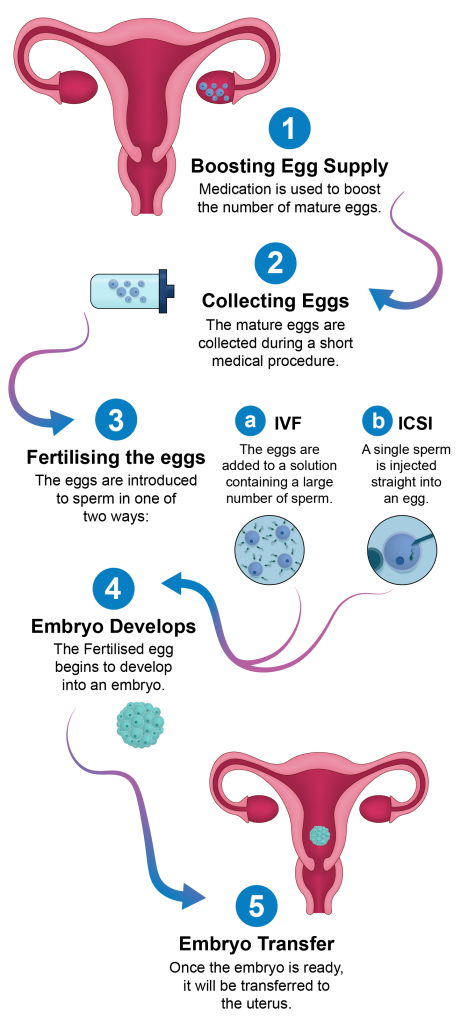
IVF cycle diagram
The picture displays a uterus with eggs in the right ovary.
1. Boosting egg supply: Medication is used to boost the number of mature eggs.
2. Collecting eggs: The mature eggs are collected during a short medical procedure. (A graphic displays eggs within a test tube.)
3. Fertilising the eggs: The eggs are introduced to sperm in one of two ways.
a. IVF: The eggs are added to a solution containing a large number of sperm. (A graphic shows four eggs each surrounded by numerous sperm.)
b. ICSI: A single sperm is injected straight into an egg. (A graphic shows a single sperm being injected into the egg.)
4. Embryo develops: The fertilised egg begins to develop into an embryo. (A graphic displays an embryo.)
5. Embryo transfer: Once the embryo is ready, it will be transferred to the uterus.
Picture displays a uterus with
Further information
To find out a bit more about difficulties conceiving and IVF and ICSI, try some of the websites below:
NHS infertility NHS IVF Fertility Network NHS trying to get pregnant NHS improve your chances of becoming a dad Tertiary Fertility Services